Did you know that accurate pathology billing can directly impact a lab’s financial stability, with Medicare payments set to decrease by 2.4% in 2025?
Pathology medical billing is essential for labs to ensure they are properly reimbursed for their services. As of 2025, the global medical billing outsourcing market is projected to reach $39.98 billion, driven by the growing complexity of billing processes and the demand for specialized expertise.
In 2025, the medical payment for the pathology lab will face a 2.4 % decrease, continuing a trend of reduced reimbursement rates since 2021. Additionally, the 2025 CPT codebook has introduced over 270 new codes, including 101 related to genetic testing and digital pathology, further complicating billing practices.
What is pathology medical billing?
Pathology medical billing is the process of submitting claims to insurance companies for laboratory services such as diagnostic tests and tissue samples. Laboratories provide CPT (Current Procedural Terminology) codes to describe the services rendered by them. Proper coding is crucial to the billing process to ensure labs get reimbursed correctly.
At the core of medical pathology billing, it is important that the billing is done appropriately to have a steady cash flow and to avoid claim denials.
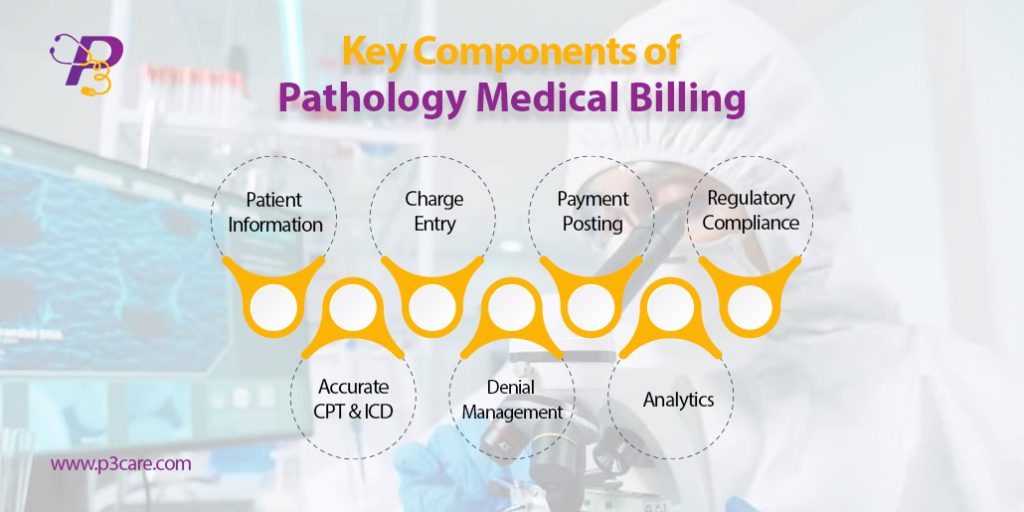
Key Components of Pathology Medical Billing
To ensure maximum reimbursement and error-free claims, it’s crucial to understand the building blocks of pathology medical billing. These components are essential for labs and billing teams to streamline the revenue cycle and reduce claim denials.
1. Patient Information & Eligibility Checks
Accurate demographic entry and insurance verification are foundational. Even minor errors in patient data can lead to rejections or underpayments.
According to MGMA, nearly 24% of denied claims result from eligibility-related mistakes.
2. Clinical Documentation & Test Requisitions
Each pathology test must be properly documented with the ordering provider’s signature, ICD-10 diagnosis codes, and proof of medical necessity.
3. Accurate CPT & ICD-10 Coding
Applying up-to-date pathology CPT coding guidelines is critical. Coders must understand distinctions between technical and professional components and use modifiers such as -26 and -TC correctly.
4. Charge Entry & Claims Submission
Clean claims—those free of errors—are submitted electronically. This accelerates approval and minimizes delays.
5. Denial Management & Appeals
Having a system in place to track, appeal, and correct denied claims ensures labs don’t lose revenue due to avoidable issues.
6. Payment Posting & Reconciliation
Every Explanation of Benefits (EOB) must be matched with charges, ensuring payments are posted correctly and underpayments are flagged.
7. Regulatory Compliance
Regulations from HIPAA, CMS, CLIA, and PAMA must be followed rigorously. Labs should conduct periodic audits to stay compliant.
8. Analytics & KPI Monitoring
Monitoring KPIs like clean claim rate, Days in A/R, and denial trends helps improve long-term performance.
Key Components of Pathology Medical Billing
Billing Services for Pathology Labs
Billing services for pathology labs go far beyond basic claim filing. These services are designed to handle high-volume lab operations while ensuring accuracy, compliance, and faster cash flow.
What’s Included in Pathology Billing Services?
- Specialized CPT and ICD-10 coding for lab tests
- Integration with LIS and EMR systems
- Claim scrubbing and compliance checks
- Real-time analytics dashboards
- Denial and appeal management
Labs that use professional billing services see a 20–30% increase in claim approval rates.
Benefits to Labs:
- Reduce in-house administrative burden
- Accelerate revenue cycles
- Improve payer compliance
- Minimize coding and billing errors
By partnering with a provider that specializes in billing services for pathology labs, labs gain a competitive edge and peace of mind.
Pathology CPT Coding Guidelines
Following the correct pathology CPT coding guidelines is non-negotiable. Every test billed must match the correct CPT and ICD-10 code, especially when working with government and commercial payers.
Key CPT Coding Guidelines for Pathology:
- Understand the difference between:
- Clinical pathology codes (e.g., 85025 – CBC with differential)
- Anatomical pathology codes (e.g., 88305 – tissue examination)
- Use appropriate modifiers:
- -26: Professional Component
- -TC: Technical Component
- -59: Distinct Procedural Service
- Apply NCCI edit rules to avoid billing bundled services separately
Stay up to date with annual changes. The 2025 CPT code updates will impact certain molecular pathology and lab panel services.
Accurate coding not only protects your revenue but also shields your lab from audits and compliance violations.
Outsourced Pathology Billing Companies
Many pathology groups and labs are now turning to outsourced pathology billing companies to reduce costs, improve collections, and stay compliant in a complex billing landscape.
Key Services Offered:
- Full revenue cycle management (RCM)
- CPT and ICD-10 coding
- Denial tracking and appeals
Reporting and trend analysis
P3care is trusted outsourced pathology billing company, which means focus on your core operations or lab testing and patient care, while the experts handle your billing.
Trends and Facts in Pathology Medical Billing (Today’s Insights)
The world of pathology medical billing is evolving rapidly. New technologies, stricter compliance standards, and changing payer behavior are all reshaping how pathology labs manage their revenue cycles.
Key Trends:
- Increased Claims Scrutiny: Payers are closely reviewing pathology claims, particularly for molecular and high-cost tests.
- Shift to Digital Pathology: Telepathology and digital slide analysis are growing, but billing guidelines are still catching up.
- AI-Powered Billing: Automation is now helping labs reduce errors and accelerate claims processing.
- Emphasis on Compliance: Labs are investing more in audits and coder education to avoid penalties.
- Rise of Outsourcing: Many labs now use an outsourced pathology billing company to ensure billing accuracy and compliance.
Fact: Labs using AI in their billing process reported a 25–30% reduction in claim denials (HFMA 2024).
2025 Pathology CPT Code Updates
Every year, CPT coding changes have a direct impact on billing operations. The 2025 CPT code updates for pathology introduce new codes, retire outdated ones, and adjust descriptors to better reflect current lab practices.
What’s New in 2025:
- Molecular Testing: Additional codes for infectious disease panels and pharmacogenomic testing.
- Digital Pathology Add-ons: New codes for remote image review and digital storage workflows.
- Clarified Descriptors: Several ambiguous codes updated for better accuracy.
AI Integration in Billing
AI is no longer the future—it’s now actively transforming clinical pathology billing solutions across the industry.
How AI Supports Pathology Billing:
- Auto-generates CPT code suggestions based on test data.
- Predicts and flags high-risk claims before submission.
Automates payment posting and EOB reconciliation.
Why It Matters:
- Improves billing accuracy.
- Reduces operational costs.
- Speeds up reimbursement cycles.
Insight: AI adoption in pathology billing is projected to grow 40% per year through 2027
Industry Statistics
Here are some current statistics that highlight the state of pathology billing in 2024–2025:
- 28% of pathology claims are denied due to coding or modifier errors.
- 45% of labs are now using some form of billing automation or AI.
- 35% of pathology practices have fully outsourced their billing operations.
Average Days in A/R for high-performing labs: 25 days (vs. industry avg. 42 days).
Conclusion
Pathology medical billing is more than a back-office function—it’s a core revenue driver. With constant changes in CPT codes, payer policies, and compliance regulations, pathology labs need to stay informed and proactive. P3Care manages billing in-house or works with an outsourced pathology billing company. Investing in technology, training, and expert support is the key to long-term financial health.
Frequently Asked Question
Q1: Why is pathology medical billing so complex?
A: It involves managing both clinical and anatomical codes, applying correct modifiers, adhering to ever-changing payer rules, and justifying medical necessity. These layers of complexity make billing accuracy and compliance a constant challenge for labs.
Q2: What are the top reasons pathology claims get denied?
Q2: What are the top reasons pathology claims get denied?
A: Common reasons include incorrect CPT codes, mismatched diagnosis codes, missing modifiers, and insufficient documentation. Regular coding audits and continuous staff training are essential to reducing denials.
Q3: How often should pathology labs update their billing and coding practices?
A: At least once a year, especially after the AMA releases CPT code updates. However, quarterly reviews are recommended to keep up with payer-specific changes and evolving compliance guidelines.
Q4: Should smaller labs outsource their billing operations?
A: Yes, outsourcing can significantly reduce administrative burden, improve cash flow, and ensure compliance. A trusted partner like P3Care helps streamline the process with certified coders and real-time reporting tools.
Q5: How does outsourcing improve billing performance?
A: Outsourcing to experienced billing professionals enhances claim accuracy, reduces denial rates, and speeds up reimbursements. It also allows labs to focus on testing and diagnostics while companies like P3Care handle the financial side.